At Home Covid Tests Education
Other ways to shop at-home COVID-19 tests
Frequently asked questions
Why should a customer consider purchasing an at-home COVID-19 test versus going to a local testing site for free?
These tests provide convenient at-home testing intended for use by individuals with or without symptoms. These options provide customers with access to testing that can be conducted at home and complement the CVS Health® commitment to providing consumers with access to comprehensive COVID-19 testing services.
What is the difference between PCR and antigen tests?
A PCR (polymerase chain reaction) test is a type of molecular test that often requires a patient sample to be sent to a lab for analysis. Getting results can take anywhere from several hours to days after being received at the lab. A PCR test can sense low levels of viral genetic material (e.g., RNA), so these tests are usually highly sensitive, which means they are good at detecting a true positive result.
An antigen test, or rapid antigen test, detects viral proteins and provides results in less than an hour. Antigen tests tend to be less sensitive than molecular tests, but you are able to get results more quickly.
You may purchase your own antigen test or PCR test to perform yourself at home. The at-home PCR test sample has to be mailed to a lab for analysis.
What is an Emergency Use Authorization (EUA)?
The United States FDA has made at-home COVID-19 tests available under an emergency access mechanism called an Emergency Use Authorization (EUA). The EUA is supported by the Secretary of Health and Human Services' (HHS) declaration that circumstances exist to justify the emergency use of diagnostics (IVDs) for the detection and/or diagnosis of the virus that causes COVID-19. An IVD made available under an EUA has not undergone the same type of review as an FDA- approved or cleared IVD. The FDA may issue an EUA when certain criteria are met, which includes that there are no adequate, approved, available alternatives, and based on the totality of scientific evidence available, it is reasonable to believe that this IVD may be effective in diagnosing COVID-19. The EUA for this test is in effect for the duration of the COVID-19 declaration justifying emergency use of IVDs, unless terminated or revoked (after which these tests may no longer be used).
What is COVID-19 serial testing?
COVID-19 serial testing occurs when one person tests themselves multiple times for COVID-19 on a routine basis, such as every day or every other day. By testing more frequently, you may detect COVID-19 more quickly and reduce spread of infection.
Are at-home COVID-19 tests free?
On Jan. 10, 2022, the Federal Government announced guidance requiring commercial insurance companies and group health plans to cover the cost of at-home diagnostic tests, also known as over-the-counter (OTC) COVID-19 tests, without involvement of a health care provider.
Below are details outlined in the guidance, which became effective on January 15, 2022:
Health plans are required to cover a maximum of eight (8) at-home COVID-19 tests without a prescription. For at-home COVID-19 test kits that contain two (2) tests per kit, a maximum of four (4) kits every 30 days are covered.
Health plans are required to have a reimbursement process for members purchasing at-home tests (up to the limit), whether purchased online or in-person.
A plan may also choose to establish a process for upfront direct coverage if members can purchase the at-home tests through the plan’s network of pharmacies and retailers.
If a plan has both a network of pharmacies/retailers and a direct-to-consumer shipping program, the plan may limit post-service reimbursement for at-home tests purchased at non-preferred providers to $12 per test.
Beginning April 4, 2022, Medicare beneficiaries enrolled with Medicare Part B or Medicare Advantage can obtain eight (8) at-home COVID-19 tests every 30 days at no out-of-pocket cost at the pharmacy counter at most CVS Pharmacy locations, including those within Target stores, following a new CMS initiative.
How are the tests paid for?
CVS Pharmacy offers several options for patients to access at-home COVID-19 tests through your prescription benefit plan. Because processes may differ across commercial, Medicare and Medicaid plans, patients should also contact their insurance provider to confirm the coverage policy and claims submission process.
Commercial and Group Health Plans:
1. Digital Option with no upfront cost:
CVS Pharmacy patients with eligible commercial or group health insurance can visit CVS.com or the CVS Pharmacy app to utilize a digital service that simplifies the process for locating, ordering, and picking up at-home COVID-19 test kits with zero upfront out-of-pocket cost and without the need for the patients to submit a claim to their health insurance provider. To check availability and order tests, patients should:
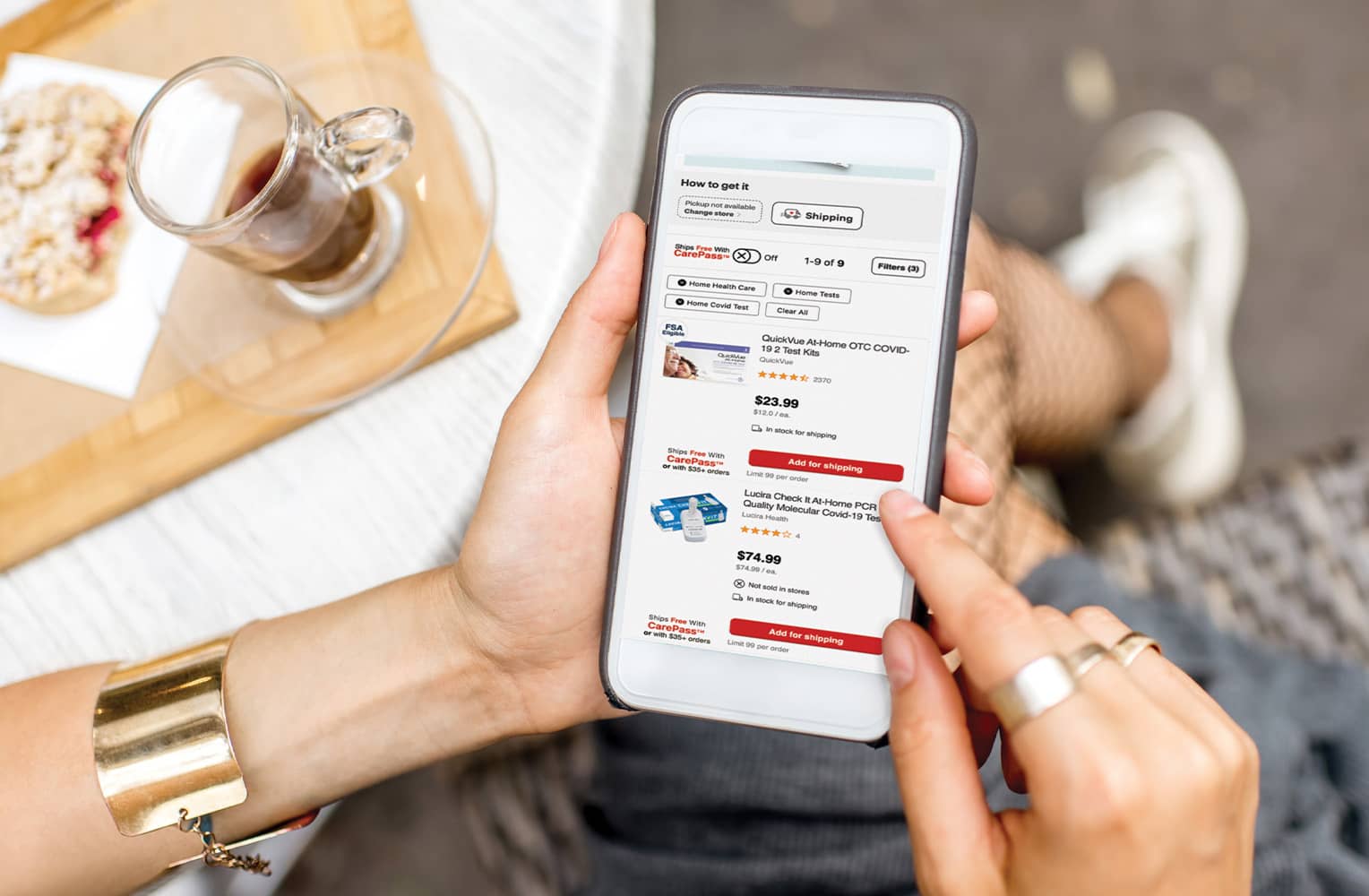
Visit CVS.com or use the CVS Pharmacy app to search for at-home COVID-19 tests at nearby CVS Pharmacy locations
Select a nearby CVS Pharmacy with tests available, then enter prescription insurance information (use ID cards that display RX BIN, RX PCN information)
Provide an email and phone number to receive notifications with updates on their order status
Head to the CVS Pharmacy they selected for fast and easy store pickup using their name and order number at the front checkout
For security purposes, CVS.com patients will be asked to log in to their account. New customers are required to register for a CVS.com account prior to providing their insurance information.
2. Pay Today and Get Reimbursed:
Patients who may be ineligible for advance reimbursement, or patients who choose to purchase pay for the kits upfront and submit receipts directly to their insurer may:
Order at-home COVID-19 test kits for delivery through CVS.com or the CVS Pharmacy app pay today and get reimbursed option; or
Visit a local CVS Pharmacy and purchase test kits directly at the checkout at the front of the store
Patients are strongly encouraged to save their receipt(s) as they may need to submit them to their insurer.
3. Request OTC Test Kits through your insurance at the CVS pharmacy counter:
Members of participating commercial insurance plans may access tests with no up-front cost by visiting the pharmacy counter at their local CVS Pharmacy. Please remember to bring your pharmacy benefit ID card(s). Look for the cards that contain the RX BIN and RX PCN information.
Medicare Part B and Medicare Advantage Plans:
Members of these plans may access tests at no up-front cost by visiting the pharmacy counter at their local CVS Pharmacy and presenting their Medicare Beneficiary ID card (red/white/blue) and/or Medicare Advantage ID card.
Medicaid Fee for Service and Managed Care Plans:
Please contact your insurer to confirm program coverage policy as many state Medicaid programs require a prescription from your medical provider.
What if I have Medicare/Medicaid?
Effective April 4, 2022, Medicare will cover up to eight (8) at-home COVID-19 tests per person every 30 days or four (4) two-test, rapid antigen at-home tests every 30 days without a prescription. Coverage is available for members eligible with Medicare Part B FFS or Medicare Advantage Benefits. Please visit your local CVS Pharmacy or request-at-home tests be billed to Medicare Part B FSS Program. You must provide your Medicare Beneficiary ID (MBI) from your Medicare red, white, or blue card. Some Medicare Advantage plans maybe also provide coverage under the Part B or Enhanced OTC benefits, please check with your Medicare Advantage plan for coverage details.
If you are a Medicaid member, please note that state policies vary as to whether a prescription is required. Please check with your insurer about coverage for at-home COVID-19 tests.
When ordering online for store pickup, where do I go for my order?
Online orders of at-home test kits will be available in dedicated locations at the front of store checkout at CVS Pharmacy, and each location will be clearly marked when entering the store. Consumers may proceed to the front of store checkout and provide their name and order number to retrieve their order.
Can I pick up my order at the drive-thru?
At this time at-home COVID-19 test orders may only be picked up inside our stores.
How long do I have to pick up my order?
Consumers will have 72 hours from when the order is placed to pick up their order.
Are CVS Pharmacy locations within Target and Schnucks included?
Eligible patients with commercial health plans and Medicare may present their prescription insurance information at CVS Pharmacy locations within Target to obtain tests. CVS Pharmacy locations inside Schnucks are not participating at this time.
Can I order online and have my tests delivered?
Yes. Customers with participating commercial health plans have the option to order tests through CVS.com or the CVS Pharmacy app and have them delivered for a fee. Delivery is free for CarePass members.
What if my local store does not have inventory?
We have worked with our vendors to significantly increase the amount of inventory of at-home COVID-19 tests. Consumers will be given a choice of nearby pharmacies with inventory during the online ordering process.
How can consumers without insurance get at-home COVID-19 test kits?
Consumers without insurance can go to CVS.com, place an order to pay out-of-pocket for tests, and have them delivered. Consumers can also purchase directly and pay out-of-pocket at a participating CVS Pharmacy.
The Federal government is also offering free at-home COVID-19 tests through mail delivery. More information on this program can be found at www.COVIDtests.gov.
What information will I need to provide to order the at-home tests?
To obtain tests digitally with no up-front cost, patients with commercial or group health insurance will need to provide:
Their prescription insurance information (RX BIN, RX PCN, RX Group, Cardholder ID)
Name
Date of birth
Number of desired tests
Desired pick-up location.
Are digital claims run through the prescription benefit or medical benefit?
Digital claims are run through the patient's commercial or group health plan prescription benefit.
I received a message that my insurance was unable to be billed. What are my options?
Consumers will be notified of their available options if their insurance is unable to be billed. Depending on availability, options may include either paying out-of-pocket at their local CVS Pharmacy or paying out-of-pocket and having the tests delivered. Consumers are also encouraged to contact their insurance provider to discuss reimbursement options. The Federal Government is also offering free at-home COVID-19 tests through mail delivery. More information on this program can be found at www.COVIDtests.gov.
How many tests are covered?
Most commercial and group health plans are required to cover a maximum of eight (8) at-home COVID-19 tests without a prescription. For at-home COVID-19 test kits that contain two (2) tests per kit, a maximum of four (4) kits every 30 days are covered.
Medicare will cover up to eight (8) at-home COVID-19 tests without a prescription within a 30 day calendar period.
Medicaid program policies differ per state. Please refer to your insurer for coverage policy details.
Does CVS Pharmacy have product limits for COVID-19 at-home tests?
At this time, we do not have limits on at-home COVID-19 tests in our stores or online.
What if I have a prescription for a test?
Patients with a prescription for an at-home COVID-19 test should go to the CVS pharmacy counter as they would any other prescription. Patients without a prescription should purchase at-home COVID-19 tests at the front of store checkout.
Are at-home COVID-19 tests eligible for returns at CVS stores?
No. All at-home COVID-19 test kit sales are final.
Are at-home COVID-19 tests HSA/FSA eligible?
At-home COVID-19 tests may be HSA/FSA eligible; however, coverage is determined by individual insurance companies. Please contact your insurer to confirm coverage.
Are at-home COVID-19 tests eligible for promotions and coupon discounts?
At-home COVID-19 tests are excluded from all coupon discounts and promotions, including CarePass® and ExtraBucks Rewards®.
If I already ordered at-home COVID-19 tests from another source (Federal program, at another store location, etc.) can I still receive tests from CVS Pharmacy as well?
Consumers are encouraged to check with their insurer to determine how many remaining tests may still be eligible for reimbursement this month. Consumers paying out-of-pocket and not through their health insurance plan can purchase as many at-home COVID-19 tests as they would like.
I have trouble ordering online. Is that the only option for ordering the at-home COVID-19 tests from CVS Pharmacy?
In order to accommodate various patient needs, CVS Pharmacy offers the following options to obtain at-home COVID 19 test kits:
Digital Options:
Order digitally and have tests delivered
Order digitally and pick up in store
Order digitally, pay upfront and get reimbursed CVS Pharmacy Options:
Local CVS Pharmacy front store purchase and get reimbursed
Local CVS Pharmacy in-pharmacy insurance claim (in-pharmacy claim required for Medicare and Medicaid plans)
As inventory and options can vary by location, we suggest patients check availability online before heading into a store location if possible.
*FOR COVID-19 HOME TEST SELECT INSURANCE CLAIM: Applies to most fully-insured and self-insured group and individual coverage, including FEHB plans until the end of the public health emergency. This also applies to Medicare and Medicaid plan coverage. Covers up to eight (8) rapid antigen single-test kits or four (4) rapid antigen two-test kits per month. COVID-19 home test kit returns will not be accepted. At-home COVID-19 tests are excluded from all coupon discounts and promotions, including CarePass® and ExtraBucks Rewards®.